Blog
Safeguarding Your Child's Eyesight
- Details
- Written by: Premier Eyecare
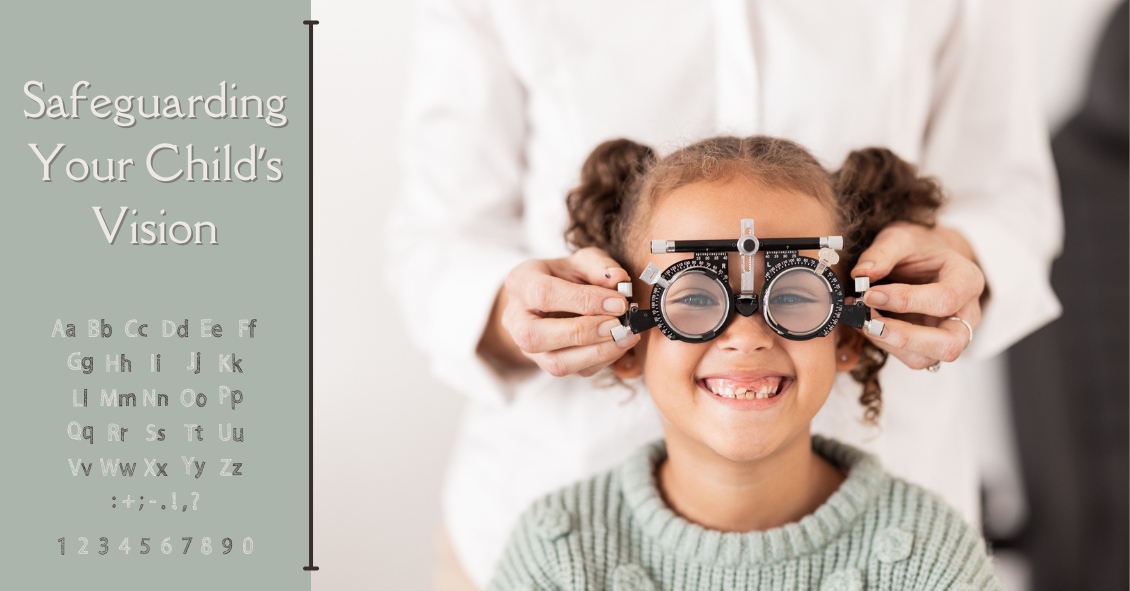
Just like adults, children need to have their eyes examined. This need begins at birth and continues through adulthood.
Following are common recommendations for when a child needs to be screened, and what
Sunglasses Are a Fabulous Investment
- Details
- Written by: Premier Eyecare

The sun does some amazing things. It plays a role in big helping our bodies to naturally produce Vitamin D. In fact, many people who work indoors are directed to take Vitamin